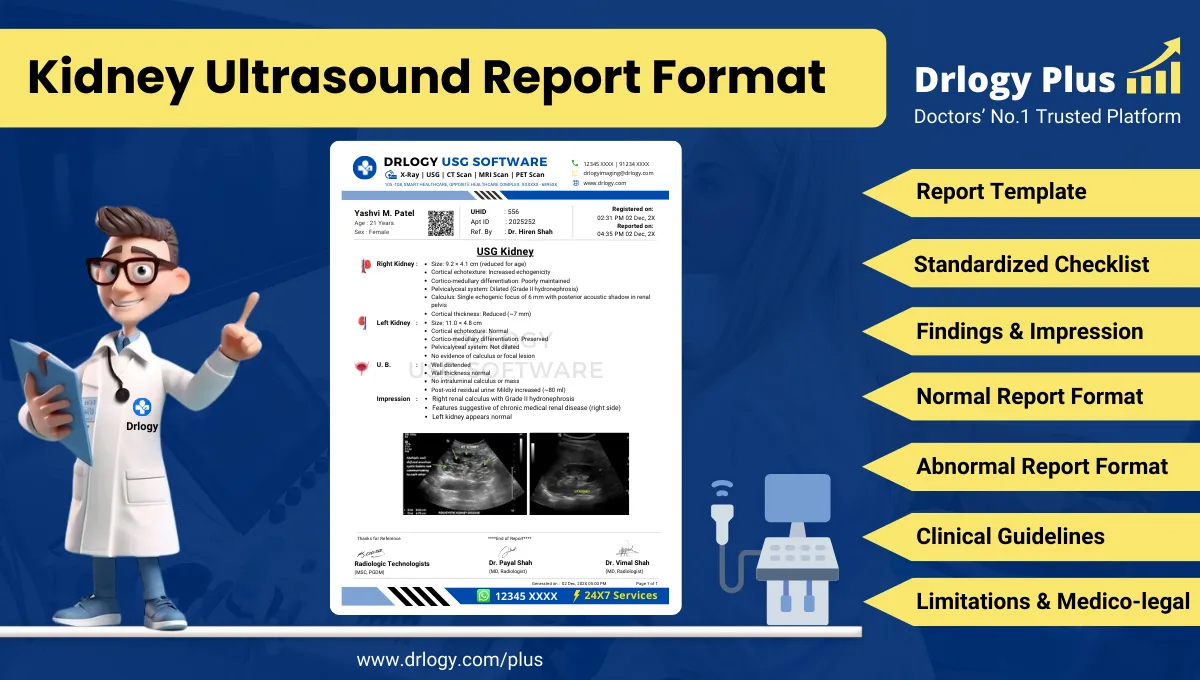
What Is a Kidney Ultrasound Report Format?
A Kidney ultrasound report format is a standardized structure for documenting renal ultrasound technique, findings, and impression with consistent terminology and measurement logic.
It supports diagnosis, referral decisions, follow-up planning, and longitudinal comparison across serial studies, particularly for obstruction, parenchymal disease, and focal lesions.
It is a medico-legal record defining examination scope, technical adequacy, observations, conservative interpretation, and stated limitations within accepted radiology reporting standards.
Check:
Explore the Best AI-Based Ultrasound Reporting Software for Radiologists
Clinical Importance of a Standardized Kidney Ultrasound Report Format
- Diagnostic clarity by ensuring uniform documentation of renal size, cortical thickness, corticomedullary differentiation, echogenicity, pelvicalyceal system, and urinary tract findings.
- Inter-doctor communication by using consistent descriptors for hydronephrosis, calculi, cystic lesions, and renal parenchymal changes that clinicians can interpret reliably.
- Reporting consistency by reducing variation in grading obstruction, measuring renal dimensions, and describing lesion morphology across radiologists and sites.
- Patient safety by reducing omission errors in high-volume settings, including missed laterality, missed PCS assessment, or incomplete documentation of ureteric/UVJ relevance when visible.
- Medico-legal protection by documenting technique, limitations (bowel gas, obesity, incomplete bladder distension), and conservative impressions aligned with ultrasound capability.
A standardized format improves completeness, reproducibility, and audit readiness for routine renal ultrasound reporting.
Why Manual Reporting Often Fails to Maintain Standardization at Scale
- Inter-radiologist variability in describing renal echogenicity, corticomedullary differentiation, and obstruction severity reduces follow-up comparability.
- Missed sections in high-volume settings commonly affect documentation of cortical thickness, ureteric jet relevance, post-void status, or ancillary findings.
- Terminology inconsistency (mild fullness vs mild hydronephrosis vs pelviectasis) creates interpretive ambiguity for referring clinicians.
- Audit challenges arise because free-text reports are difficult to benchmark, search, and quality-check against standard renal reporting elements.
Software-assisted structured reporting improves completeness and uniformity without altering radiologist responsibility or clinical judgment.
Indications for Kidney Ultrasound
- Flank pain with suspected renal/ureteric obstruction
- Hematuria evaluation (gross or microscopic) as clinically indicated
- Renal function impairment with suspected obstructive uropathy or parenchymal disease
- Follow-up of known hydronephrosis or hydroureteronephrosis
- Suspected renal calculi or recurrent stone disease monitoring
- Hypertension work-up where renal morphology assessment is requested
- Recurrent urinary tract symptoms with suspected upper tract involvement
- Screening or follow-up of renal cysts or known focal renal lesions
- Post-intervention or post-surgical follow-up (stent, nephrostomy, transplant context if specified)
A concise indication focuses the report on clinically relevant renal questions and improves impression utility.
Pre-Examination Details to Be Documented
Kidney ultrasound reporting should begin with complete pre-examination documentation to preserve interpretive accuracy and medico-legal defensibility.
- Patiententifiers: full name, age, sex, unique, accession/study number, study date and time.
- Referral details: referring clinician, specialty/department, and clinical question (obstruction, stones, cyst follow-up, renal size/parenchyma).
- Clinical notes: laterality of pain, fever, prior stone history, known CKD, prior imaging summary and date if available, relevant labs if provided (creatinine, urinalysis), pregnancy status when relevant to urinary symptoms context.
- Preparation status: hydration/bladder filling status if pelvis/UVJ or post-void assessment is intended; fasting not mandatory for kidney-only scan but note any limitations affecting windows.
- Safety checks: correct patient verification, correct study labeling (right/left), documentation of any procedural context (post-stent, post-nephrostomy) when applicable.
How Reporting Software Ensures Complete Pre-Examination Documentation
Structured reporting systems support consistent renal ultrasound documentation through workflow controls designed for high-volume practice.
- Mandatory field enforcement ensures patiententity, laterality, indication, and key clinical notes are completed before finalization.
- Safety checklist compliance standardizes correct-patient checks, right/left confirmation, and documentation of preparation status when urinary bladder evaluation is relevant.
- Clinical note traceability links referral indications, prior imaging references, and comparison statements to the report, supporting longitudinal interpretation.
- Renal template prompts reduce omission of standard renal fields such as renal length, cortical thickness, corticomedullary differentiation, PCS status, and focal lesion characterization.
- Implementation example: Drlogy Radiology Reporting Software can be configured to apply kidney ultrasound templates with mandatory renal fields and standardized phrasing controls for impressions and limitations.
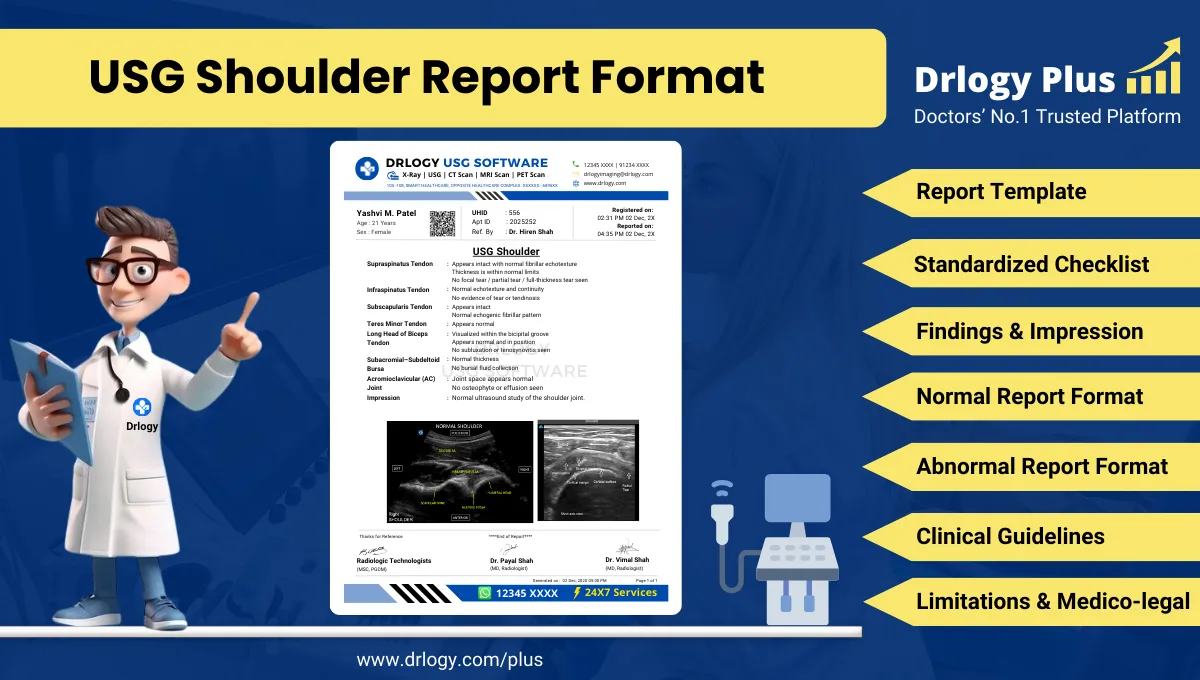
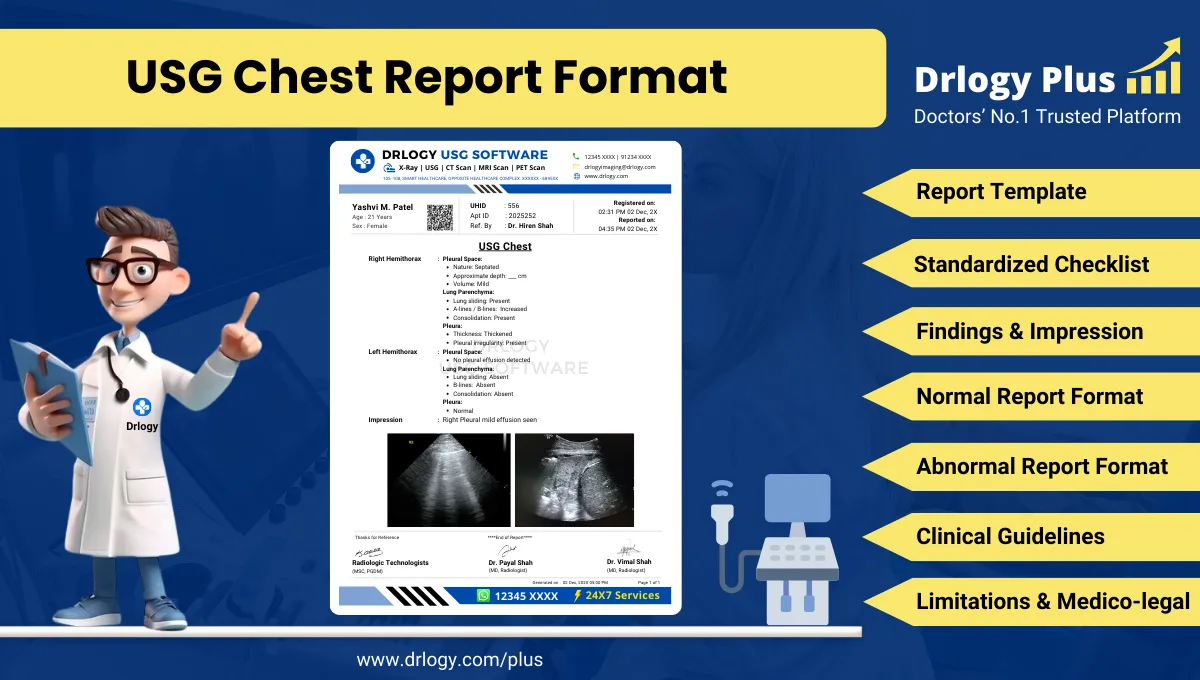
Standard Sections of a Kidney Ultrasound Report Format
A professional kidney ultrasound report format generally includes:
- Patient & Study Information
- Clinical History / Indication
- Technique / Protocol
- Findings (structured renal and urinary tract assessment, as applicable)
- Impression / Conclusion
- Limitations of the Study
- Recommendations & Follow-Up (if applicable)
Consistent section order improves readability, reduces omissions, and supports audit workflows.
Patient & Study Information Section
This section should establish traceability and medico-legal completeness:
- Patient demographics (name, age, sex) and uniqueentifier
- Study date and time, accession/study number, facility/location
- Referrer name and specialty/department
- Examination name and scope: kidney ultrasound (and bladder/post-void or Doppler if performed)
- Prior studies for comparison: modality and date if available
- Report authorization: reporting radiologistentification and timestamp as per institutional workflow
Clinical History / Indication Section
The clinical history should be concise andectly relevant:
- Primary symptom or clinical question (flank pain, hematuria, CKD, suspected obstruction)
- Relevant past history (stone disease, recurrent UTI, known hydronephrosis, known cyst/lesion, renal surgery)
- Device/procedural context if present (stent, nephrostomy catheter)
- Comparison request and prior imaging context if provided
Avoid speculative clinical narratives; document only provided or verified referral information.
Technique / Protocol Section
Technique should reflect real-world ultrasound documentation standards and clarify scope.
- Positioning: supine; lateral decubitus or prone as required for acoustic windows.
- Views: longitudinal and transverse views of each kidney; focused views of renal pelvis and proximal ureter when visible; bladder/UVJ evaluation when included.
- Transducer: curvilinear probe appropriate for depth; linear probe for superficial lesions as needed.
- Doppler: color/spectral Doppler usage documented when performed (renal perfusion assessment, suspected vascular complication, resistive indices if requested in specific contexts).
- Bladder evaluation: if included, document bladder distension adequacy; pre-void and post-void assessment if performed; note ureteric jets if evaluated.
- Measurements: document renal length; additional dimensions and cortical thickness per institutional preference; lesion dimensions in three planes when feasible.
Technique documentation supports interpretive defensibility, especially when limitations affect sensitivity.
Findings Section – Organ/System-Wise Reporting
Renal ultrasound findings should be objective, structured, and reproducible. A high-quality kidney ultrasound report format typically documents right kidney, left kidney, and any included urinary bladder/ureteric findings in a consistent sequence.
Right Kidney
Document the following elements systematically:
- Location and visualization: adequately visualized vs partially obscured; note if ectopic position suspected or if visualization is limited.
- Size: renal length (cm) with interpretation as within expected range vs reduced/enlarged, using conservative language and clinical correlation when needed.
- Cortical thickness: measured or described (preserved vs reduced), noting that thresholds may vary and should be interpreted in clinical context.
- Corticomedullary differentiation (CMD): preserved vs reduced; describe objectively without asserting etiology.
- Parenchymal echogenicity: normal vs increased echogenicity relative to liver/spleen where appropriate; describe heterogeneity if present.
Collecting system:
- No pelvicalyceal dilatation, or
- Pelviectasis / hydronephrosis description with laterality and conservative grading (mild/moderate/severe) based on institutional conventions.
- Document calyceal involvement and cortical thinning if present, and avoid overstatement when grading is limited by bladder status or hydration.
- Renal sinus: echogenicity, sinus lipomatosis description if notable (avoid definitive labeling unless supported).
Calculi:
- Location (upper/mid/lower calyx, pelvis), size, echogenic focus with posterior acoustic shadowing; twinkle artifact mention if used; note if no shadowing and therefore indeterminate.
- If multiple, describe representative stones and overall distribution.
Focal lesions:
- Cystic lesions: size (three dimensions), wall, septations, internal echoes, calcification, posterior enhancement; describe complexity without definitive Bosniakification unless institutional policy supports cautiousification with correlation.
- Solid lesions: size, echogenicity, margins, vascularity on Doppler if assessed; emphasize limitation of ultrasound for characterization.
Perinephric region: perinephric fluid/collection; fat stranding is notectly assessed on ultrasound, so avoid CT-style descriptors; document only visible fluid/collection.
Left Kidney
Useentical structured fields to reduce asymmetry in reporting:
- Visualization and position
- Size and comparative comment if relevant (right vs left)
- Cortical thickness and CMD
- Parenchymal echogenicity and echotexture
- Collecting system status and obstruction grading
- Calculi documentation
- Focal lesion characterization (cystic/solid)
- Perinephric region findings
Consistency between right and left kidney documentation is critical for follow-up comparability and audit clarity.
Ureters and Ureterovesical Junction (When Visible or When Bladder Included)
Ultrasound sensitivity for ureteric visualization varies. Document only what is assessed:
- Proximal ureteric dilatation if visualized
- Hydroureteronephrosis if present, with side and extent if determinable
- UVJ region comments if bladder included and visualization adequate
- Avoid definitive site-of-obstruction statements unless supported by clear sonographic visualization (e.g., visible distal ureteric calculus at UVJ with shadowing).
Urinary Bladder (If Included in Study Scope)
If the exam includes bladder evaluation, document:
- Distension adequacy and wall thickness assessment context (underfilled bladder limits wall assessment)
- Intraluminal findings: echogenic foci with shadowing (suggestive of calculus), mass-like lesions (describe only), debris, clots (describe, do not diagnose)
- Post-void residual volume if measured
- Ureteric jets if evaluated (presence/absence can be variable; avoid overinterpretation)
Ancillary Findings Relevant to Renal Interpretation
Document when visible and relevant:
- Ascites or free fluid (if incidentally noted)
- Pelvic masses that may contribute to obstruction (describe cautiously without definitive causality)
- Prostatic enlargement comment only if pelvis/bladder included and prostate evaluated; otherwise avoid.
Normal vs Abnormal: Reporting Discipline
Best-practice renal reporting separates objective findings from interpretive statements:
- State normal findings explicitly (e.g., “no hydronephrosis,” “no focal lesion”) to confirm completeness.
- Use standardized descriptors for echogenicity and CMD to reduce variability.
- Use conservative obstruction grading language and acknowledge factors affecting assessment (hydration, bladder filling).
- Avoid definitive etiologic statements for CKD, infection, or malignancy based solely on ultrasound patterns; use “suggestive of” and recommend correlation as appropriate.
Impression / Conclusion Section
A kidney ultrasound impression should be concise and aligned with the referral question. It should:
- Summarize key abnormalities first (obstruction, calculi, parenchymal changes, focal lesions).
- Include clinically meaningful negatives when relevant (e.g., “no hydronephrosisentified” in obstruction query).
- Use conservative medico-legal wording: “features suggestive of,” “may represent,” “correlate clinically,” “ultrasound characterization is limited.”
- Avoid definitive diagnosis for indeterminate lesions; recommend further assessment only when clinically indicated.
- When obstruction is present, describe severity and side; avoid definitive obstruction level unless clearly visualized.
- Where possible, mention comparison cautiously: “appears similar to prior study dated …” or “interval change cannot be reliably assessed” if technique differs.
The impression is a targeted summary, not a repetition of the entire findings narrative.
Limitations of the Study
- Bowel gas obscuring partial renal outline or limiting evaluation of the renal pelvis/proximal ureter.
- Patient body habitus reducing penetration and sensitivity for small calculi or small cortical lesions.
- Suboptimal patient cooperation or limited breath-hold affecting windows, especially for upper poles.
- Underfilled urinary bladder limiting UVJ evaluation, distal ureter assessment, and bladder wall interpretation (if bladder included).
- Limited ability of grayscale ultrasound to characterize indeterminate solid renal masses or complex cystic lesions definitively.
- Acoustic shadowing from ribs or adjacent bowel limiting upper pole visualization.
- Comparison limitations when prior imaging is unavailable or when prior modality differs significantly.
Limitations should be documented whenever sensitivity is reduced or characterization is inherently constrained.
Recommendations & Follow-Up (If Applicable)
- Correlate renal echogenicity/CMD changes with renal function tests and clinical history when parenchymal disease is suspected.
- Consider follow-up ultrasound when mild collecting system dilatation is present and clinical context supports surveillance, acknowledging hydration/bladder factors.
- Consider further characterization with appropriate contrast-based cross-sectional imaging when a focal renal lesion is indeterminate on ultrasound, if clinically indicated.
- Consider Doppler assessment or additional targeted ultrasound views when vascular concerns are raised but not adequately evaluated in the current study.
- Recommend review of prior imaging and correlation with clinical symptoms when interval assessment is important for known lesions or hydronephrosis follow-up.
Recommendations must remain conservative, indication-linked, and framed as options rather thanectives.
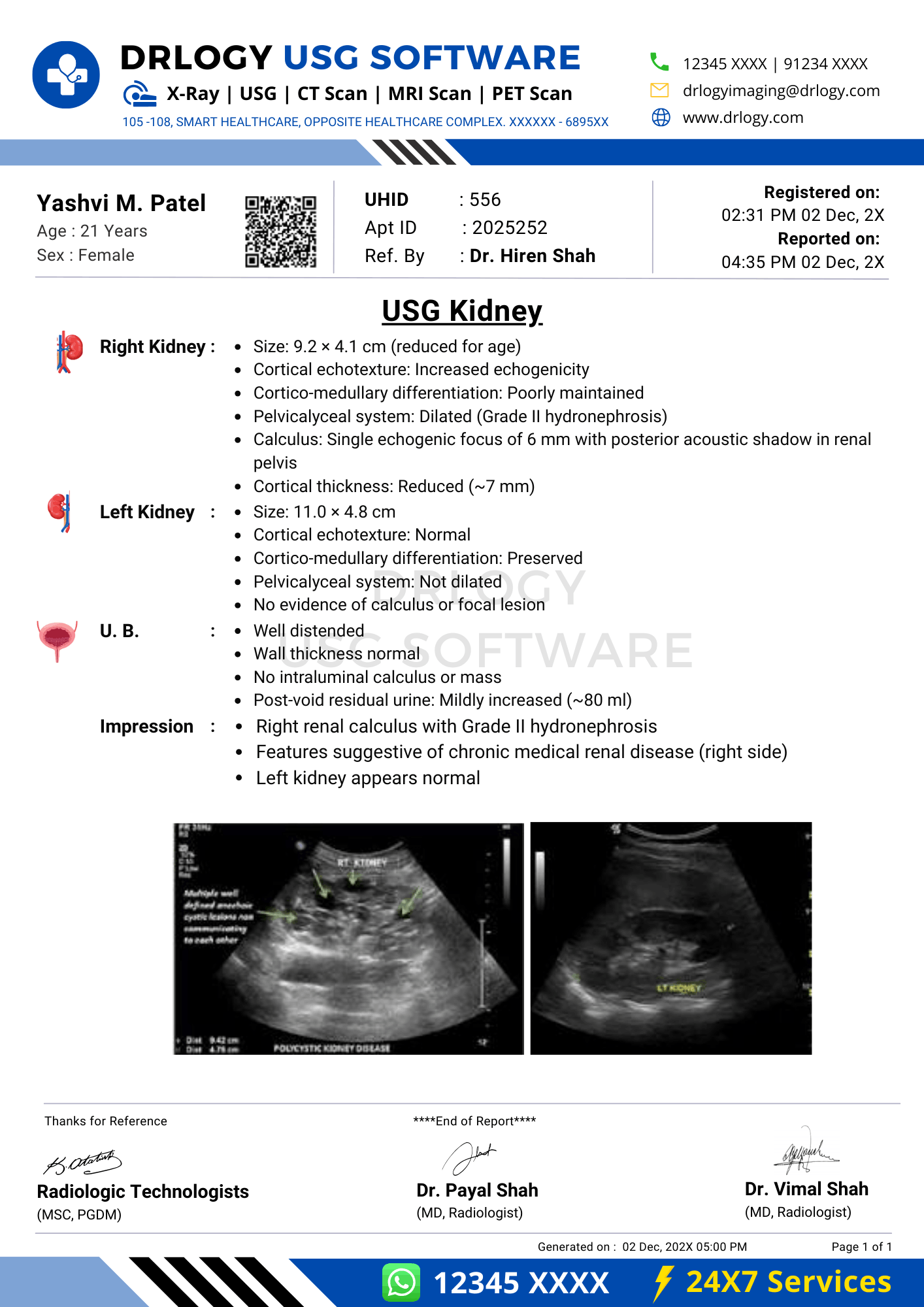
Normal Kidney Ultrasound Report Format (Sample)
Patient & Study Information:
Patient: [Name], [Age]/[Sex]
Study Date/Time: [DD-MM-YYYY, Time]
Referrer: [Clinician/Department]
Examination: Kidney Ultrasound
Clinical History / Indication:
Flank pain. Evaluate for renal obstruction or calculi.
Technique / Protocol:
Transabdominal ultrasound of both kidneys performed using a curvilinear transducer. Longitudinal and transverse views obtained. Color Doppler used for selected vascular assessment as needed.
Findings:
Right kidney is normal in size measuring [ ] cm. Cortical thickness is preserved with maintained corticomedullary differentiation. Parenchymal echogenicity is within expected limits. No pelvicalyceal dilatation is seen. No echogenic calculus with posterior shadowing isentified. No focal renal lesion is seen.
Left kidney is normal in size measuring [ ] cm. Cortical thickness is preserved with maintained corticomedullary differentiation. Parenchymal echogenicity is within expected limits. No pelvicalyceal dilatation is seen. No echogenic calculus with posterior shadowing isentified. No focal renal lesion is seen.
Impression / Conclusion:
Normal sonographic appearance of both kidneys. No hydronephrosis or renal calculusentified.
Limitations:
No significant technical limitation noted.
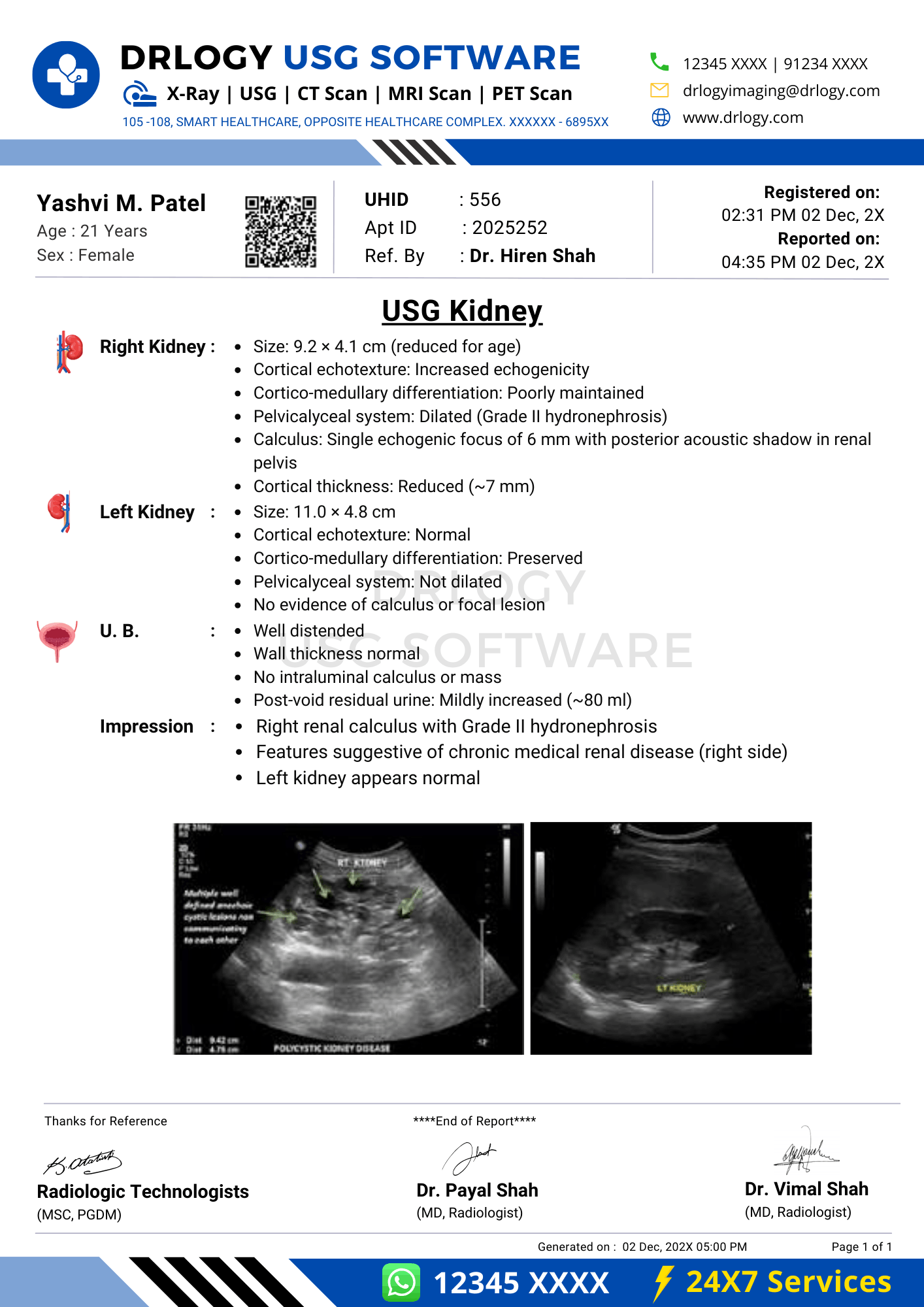
Abnormal Kidney Ultrasound Report Format (Sample)
Patient & Study Information:
Patient: [Name], [Age]/[Sex]
Study Date/Time: [DD-MM-YYYY, Time]
Referrer: [Clinician/Department]
Examination: Kidney Ultrasound
Clinical History / Indication:
Hematuria. Evaluate kidneys for calculi or focal lesions.
Technique / Protocol:
Transabdominal ultrasound of both kidneys performed. Longitudinal and transverse views obtained. Doppler assessment performed for lesion vascularity where feasible.
Findings:
Right kidney measures [ ] cm. Cortical thickness appears mildly reduced with reduced corticomedullary differentiation. Parenchymal echogenicity appears mildly increased. Mild pelvicalyceal dilatation is noted without definitive visualization of an obstructing calculus. An echogenic focus with posterior acoustic shadowing is seen in the lower pole measuring approximately [ ] mm, suggestive of a renal calculus. No perinephric collection is seen.
Left kidney measures [ ] cm. Cortical thickness and corticomedullary differentiation are preserved. No pelvicalyceal dilatation is seen. A well-defined cystic lesion is seen measuring [ ] x [ ] x [ ] cm with thin wall and posterior acoustic enhancement; no internal septations or solid component isentified on this examination.
Impression / Conclusion:
Findings suggestive of mild right-sided collecting system dilatation with renal calculus as described. Parenchymal changes of the right kidney as described; clinical and laboratory correlation is advised. Left renal cystic lesion as described.
Limitations:
Assessment for exact level of obstruction and characterization of indeterminate lesions is limited on ultrasound; technical factors may further limit sensitivity as applicable.
How Drlogy Radiology Reporting Software Standardizes These Report Formats
- Template-driven reporting ensures consistent right/left kidney documentation with mandatory fields for size, cortical thickness, CMD, echogenicity, collecting system status, and focal lesion descriptors.
- Impression safety controls support conservative wording for obstruction severity, indeterminate lesions, and parenchymal disease patterns, reducing diagnostic overstatement.
- Uniform formatting across modalities maintains continuity between USG renal findings and subsequent CT/MRI follow-up reporting by consistent terminology and section structure.
- AI-enabled reporting from scan images can assist in drafting structured content from predefined renal checklists, while maintaining radiologist verification and accountability.
- Audit-ready documentation supports completeness checks, structured QA review, and improved traceability of indications, comparisons, and limitations.
10 Key Clinical Guidelines for an Effective Kidney Ultrasound Report Format
- Document laterality explicitly and maintain a fixed order (right kidney then left kidney) to reduce reporting errors.
- Record renal length consistently and interpret size conservatively, acknowledging patient habitus and clinical context.
- Document cortical thickness and corticomedullary differentiation as separate elements to improve parenchymal assessment reproducibility.
- Use standardized echogenicity terminology and avoid etiologic conclusions without supportive context.
- Document collecting system status explicitly and grade hydronephrosis conservatively, noting factors that may influence appearance.
- For calculi, document location, size, shadowing, and ancillary sonographic signs; avoid claiming ureteric level unless visualized.
- For cystic lesions, document complexity features (wall, septations, internal echoes, calcification) and avoid definitiveification if not supported.
- Separate objective findings from impression; keep impression focused on clinically relevant conclusions that answer the referral question.
- Document relevant associated findings (perinephric fluid, bladder findings if included) that influence interpretation and management.
- Treat limitations as mandatory documentation whenever sensitivity is reduced by bowel gas, obesity, or incomplete bladder distension.
Consistent application of these guidelines improves diagnostic clarity, follow-up comparability, and medico-legal defensibility in renal ultrasound reporting.
Common Reporting Errors to Avoid
- Omission of cortical thickness or CMD documentation in suspected CKD; prevent by mandatory parenchymal fields within templates.
- Inconsistent obstruction terminology (fullness vs hydronephrosis) without stated severity; prevent by standardized grading language and defined terms.
- Incomplete calculus description (missing shadowing, location, or size); prevent by a calculi checklist in each kidney subsection.
- Overstatement of diagnosis for indeterminate masses or complex cysts; prevent by conservative impression phrasing and explicit limitations statements.
- Missing limitations despite suboptimal windows or underfilled bladder; prevent by a fixed limitations section for every report.
Avoiding these errors improves report credibility and reduces downstream clinical ambiguity.
Medico-Legal Considerations in Radiology Reporting
- Documentation safety: record objective observations and measurements; avoid unsupported statements beyond ultrasound capability.
- Disclaimers: document limitations explicitly when sensitivity is reduced; avoid implying exclusion of disease not assessable by ultrasound.
- Accountability: ensure completeentifiers, timestamps, and authorizing radiologist details per institutional policy.
- Audit readiness: maintain consistent section structure and terminology to support QA review and peer audit.
- Comparative accuracy: specify prior study date/modality and use cautious interval language when imaging conditions differ.
- Conservative impressions: use “suggestive of” and differential-level language for indeterminate findings; avoid definitive oncologic labeling.
- Record integrity: ensure version control, retention, and traceable amendments are handled according to institutional medico-legal requirements.
Medico-legal strength depends on completeness, conservative language, and transparent documentation of scope and limitations.
Structured Reporting vs Narrative Reporting
| Aspect | Structured | Narrative |
|---|
| Completeness | Standard renal fields reduce omissions in size, CMD, cortical thickness, PCS status, calculi, and lesions. | Dependent on individual habit and time; omissions more likely in high-volume reporting. |
| Consistency | Controlled terminology and fixed order improve inter-radiologist comparability and follow-up assessments. | Terminology and structure vary, complicating clinical interpretation and longitudinal comparison. |
| Audit readiness | Facilitates QA checks, benchmarking, and structured data extraction for compliance. | Difficult to audit consistently; key data may be buried or inconsistently phrased. |
| Efficiency | Templates speed routine reporting and reduce rework for missing information. | Can be fast for individuals but often requires clarifications or addenda. |
| Medico-legal robustness | Standard limitations and conservative impression controls improve defensibility. | Greater risk of ambiguous wording, missing limitations, and inconsistent documentation. |
Role of Technology in Radiology Reporting
- PACS and RIS integration supports access to images, priors, and structured reporting fields within the same workflow.
- Voice dictation improves throughput when paired with structured templates that preserve section order and completeness.
- AI-assisted formatting can prompt missing renal fields and standardize phrasing while retaining radiologist verification.
- RIS-based structured templates ensure consistent renal reporting across sites, shifts, and reporting doctors.
- Modality-specific reporting software supports kidney ultrasound templates with calculi and hydronephrosis checklists and audit-ready outputs.
Technology improves consistency and operational reliability when designed to support professional judgment.
Why High-Volume Radiology Centers Prefer Software-Based Reporting Formats
- Reduced report turnaround time through reusable templates and fewer addenda for missing elements.
- Improved quality assurance via standardized renal checklists for parenchyma, obstruction, calculi, and lesions.
- Multi-radiologist consistency across shifts and locations, enabling predictable clinician interpretation.
- Enhanced scalability as volumes rise, limiting variability and omission errors.
- Better audit readiness through structured fields, completeness validation, and standardized terminology.
- Reduced medico-legal risk through consistent limitations documentation and conservative impression controls.
- Improved longitudinal follow-up comparison by consistent measurement and wording across serial renal ultrasound reports.
Frequently Asked Questions (FAQs)
How should a kidney ultrasound report format document hydronephrosis without overstatement?
Describe collecting system dilatation objectively, grade conservatively, state laterality, and avoid declaring obstruction level unless a causative lesion isectly visualized.
What is the minimum documentation required for renal parenchymal assessment in ultrasound reports?
Renal size, cortical thickness, corticomedullary differentiation, parenchymal echogenicity, and echotexture should be documented for each kidney with conservative interpretation.
How should indeterminate renal masses be handled in the impression of a kidney ultrasound report format?
Summarize lesion morphology, acknowledge ultrasound characterization limits, and use non-definitive language; recommend further evaluation only if clinically indicated.
Which medico-legal elements should always be present in renal ultrasound reporting?
Complete patiententifiers, technique scope, right/left structure, key positives and relevant negatives, explicit limitations when present, and conservative impression wording aligned with ultrasound capability.
Does structured reporting limit radiologist flexibility compared with narrative dictation?
Structured reporting standardizes order and completeness while allowing free-text within sections for nuanced interpretation and clinically appropriate emphasis.
Key Takeaways for Radiology Professionals
- Design kidney ultrasound report formats for completeness, reproducibility, and medico-legal safety in routine clinical practice.
- Maintain a fixed right–left reporting structure, documenting renal size and parenchymal parameters consistently.
- Treat collecting system assessment as mandatory, especially when evaluating suspected obstruction.
- Use standardized terminology for echogenicity, corticomedullary differentiation (CMD), and hydronephrosis grading.
- Avoid etiologic conclusions beyond ultrasound capability; keep interpretations modality-appropriate.
- For calculi and focal lesions, document morphology, exact measurements, and location clearly, with conservative wording in the impression.
- Explicitly state limitations (e.g., bowel gas, body habitus, underfilled bladder) and leverage structured templates and tech-enabled workflows to reduce omissions, improve audit readiness, and strengthen clinician trust.
Expert Picks
View All Expert-Approved Radiology Reporting Sample Formats
Final Conclusion
A standardized Kidney ultrasound report format is essential for high-quality renal imaging communication, reliable follow-up comparison, and medico-legal defensibility across routine and high-volume diagnostic environments.
Structured reporting software supports consistent sectioning, completeness enforcement, conservative impression controls, and audit-ready documentation while preserving radiologist authority and accountability, consistent with Drlogy’s reporting workflow approach.